Human metapneumovirus (hMPV) is a globally circulating respiratory virus, and its presence has been observed in many countries, including China. Research and surveillance efforts in China have provided valuable insights into the epidemiology, transmission patterns, and clinical characteristics of hMPV.
Table of Contents
ToggleINTRODUCTION
Infection of the respiratory tract is the most common in human.Respiratory infections are caused by bacteria as well as viruses. The infection caused by the virus is the most common and they are the source of discomfort ,disability and loss of time to many adults and cause of morbidity and mortality in young children and elderly persons. Viruses like influenza,parainfluenza, respiratory syncytial virus,coronavirus etc are the causes of respiratory illness causing cold like symptoms such as running nose,sore throat,sneezing,coughing. Human metapneumovirus (hMPV) is common but lesser-known cause of respiratory infection
What is Human Metapneumovirus?
HMPV is a common type of virus that causes respiratory tract infection.The virus belong to family pneumoviridae same of respiratory syncytial virus (RSV) .The virus is not new discovered in Netherlands in 2001 by Dutch scientists team led by Dr. B. van den Hoogen at the Erasmus Medical Center.Genetic analysis revealed that hMPV was closely related to avian metapneumovirus (AMPV), suggesting an evolutionary link.
Further studies confirmed that hMPV had likely been circulating in humans for decades before its discovery, with retrospective serological studies showing evidence of infection dating back to at least the 1950s.
Taxonomy
|
Genus |
Species |
virus |
|
Metapneumovirus |
Metapneumovirus avis Metapneumovirus hominis |
avian metapneumovirus (AMPV) Human metapneumovirus (HMPV) |
HMPV and RSV genome are similar. This virus contains two main genetic lineages subtypeA and B with subtypes A1/A2 and B1/B2 respectively. HMPV having negative sense single stranded RNA viruses.
How Is Human Metapneumovirus Transmitted?
Human metapneumovirus (hMPV) spreads primarily through respiratory droplets and direct contact, similar to many other respiratory viruses. Its transmission pathways make it highly contagious, especially in settings where close interaction occurs, such as homes, schools, healthcare facilities, and crowded public spaces. Understanding its modes of transmission is essential for preventing its spread and protecting vulnerable populations.
Modes of Transmission
- Respiratory Droplets:
- When an infected individual coughs, sneezes, or even talks, tiny droplets containing the virus are expelled into the air.
- These droplets can be inhaled by others in close proximity, leading to infection.
- Transmission via droplets is most effective in indoor environments with poor ventilation.
- Direct Contact:
- Touching contaminated surfaces or objects and then touching the mouth, nose, or eyes can transfer the virus.
- Common items, such as doorknobs, toys, and shared utensils, can harbor the virus if handled by an infected person.
- Close Person-to-Person Contact:
- Close interactions, such as hugging, kissing, or caring for an infected person, can facilitate the direct transfer of the virus.
- This mode of transmission is especially significant in families and healthcare settings.
Viral Shedding and Infectious Period
- Incubation Period: The time between exposure to hMPV and the onset of symptoms is typically 3–6 days.
- Viral Shedding: Infected individuals can shed the virus even before symptoms appear and continue to do so for 1–2 weeks after the onset of illness.
- Asymptomatic Carriers: Some individuals, particularly adults with mild or no symptoms, can unknowingly spread the virus to others, contributing to its circulation.
High-Risk Scenarios for Transmission
- Seasonal Patterns:
- hMPV infections peak during late winter and early spring, coinciding with other respiratory viruses, increasing the likelihood of community spread.
- Crowded Settings:
- Schools, daycare centers, and nursing homes are hotspots for hMPV transmission due to the close contact among individuals.
- Hospitals and clinics also pose a risk, especially in pediatric wards and intensive care units.
- Poor Hygiene Practices:
- Lack of regular hand washing and improper respiratory etiquette (e.g., not covering the mouth while coughing) significantly increases transmission.
Prevention of Transmission
While no vaccine or specific antiviral treatment exists for hMPV, simple preventive measures can reduce the risk of transmission:
- Hand Hygiene: Regular washing of hands with soap and water for at least 20 seconds or using alcohol-based hand sanitizers.
- Respiratory Hygiene: Covering the mouth and nose with a tissue or elbow when coughing or sneezing.
- Surface Disinfection: Regular cleaning of frequently touched surfaces and objects.
- Avoiding Close Contact: Keeping a safe distance from individuals who are sick, especially if symptoms like coughing or sneezing are present.
- Mask-Wearing: Using masks in crowded or high-risk settings to prevent droplet transmission.
- Isolation of Infected Individuals: Encouraging those with symptoms to stay home until they recover fully.
Who Is At Risk Of hMPV Infection?
Human metapneumovirus (hMPV) can affect people of all ages, but the severity of the illness varies depending on the individual. Some groups are more likely to experience serious complications due to factors such as age, weakened immune systems, or pre-existing health conditions. Identifying these high-risk populations is essential for implementing effective prevention measures and ensuring timely medical care.
1.Infants and Young Children
- Why They Are at Risk:
- Immature immune systems make infants and young children more susceptible to infections.
- They are often exposed to hMPV in daycare centers, schools, or through contact with siblings or caregivers.
- Impact:
- hMPV is a leading cause of lower respiratory tract infections (LRTIs) in children under 5 years of age.
- Severe cases can lead to bronchiolitis, pneumonia, and respiratory distress, sometimes requiring hospitalization.
- Key Statistics:
- Studies suggest that nearly all children are exposed to hMPV by the age of 5.
2. Elderly Individuals
- Why They Are at Risk:
- Aging leads to a gradual decline in immune function, known as immunosenescence, making older adults more vulnerable to infections.
- Many elderly individuals have comorbidities, such as chronic obstructive pulmonary disease (COPD) or heart disease, which can worsen the effects of respiratory infections.
- Impact:
- Severe cases in older adults often present as pneumonia or exacerbations of pre-existing chronic conditions.
- Hospitalization rates and mortality are higher in this age group compared to healthy adults.
3. Immunocompromised Individuals
- Who Falls in This Category:
- Patients undergoing chemotherapy or organ transplantation.
- Individuals with HIV/AIDS or other conditions affecting immune function.
- People on long-term immunosuppressive medications, such as steroids.
- Why They Are at Risk:
- Impaired immune responses make it harder for the body to fight off viral infections.
- Prolonged viral shedding is common in immunocompromised patients, leading to a higher risk of severe and prolonged illness.
- Impact:
- hMPV can cause severe pneumonia, and these individuals may require intensive medical care.
4. People with Chronic Respiratory or Cardiac Conditions
- Examples of Conditions:
- Asthma, COPD, interstitial lung disease, or pulmonary fibrosis.
- Congestive heart failure or other chronic heart conditions.
- Why They Are at Risk:
- Pre-existing respiratory or cardiac conditions can exacerbate the effects of hMPV infections.
- hMPV can trigger asthma exacerbations or worsen symptoms of COPD, leading to complications.
- Impact:
- Higher likelihood of hospitalization and prolonged recovery.
5. Individuals in Close-Contact Environments
- Examples of Settings:
- Schools, daycare centers, nursing homes, and healthcare facilities.
- Why They Are at Risk:
- Crowded environments increase the risk of exposure to respiratory droplets or contaminated surfaces.
- Frequent close contact with infected individuals facilitates rapid viral spread.
- Impact:
- Outbreaks in such settings can affect large groups, particularly vulnerable individuals like children or the elderly.
6. People with Limited Access to Healthcare
- Why They Are at Risk:
- A delay in diagnosing and treating the condition can result in more serious complications.
- Poor living conditions, malnutrition, and lack of preventive care increase vulnerability to respiratory infections, including hMPV.
- Impact:
- These individuals often face higher morbidity and mortality rates due to limited medical resources.
What Are The Symptoms Of Humanmetapneumovirus(hMPV) Infection?
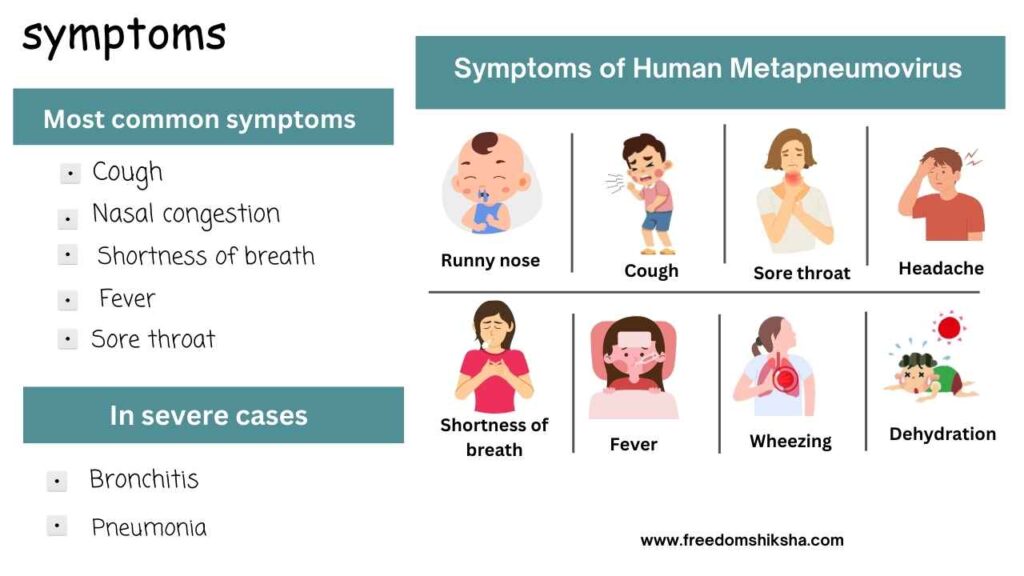
Human metapneumovirus (hMPV) can cause a wide spectrum of respiratory illnesses, ranging from mild, cold-like symptoms to severe lower respiratory tract infections (LRTIs). The severity of symptoms varies based on factors such as the patient’s age, immune status, and underlying health conditions. Here’s a detailed look at the symptoms associated with hMPV infection.
1. Mild Symptoms
In most healthy individuals, especially adults, hMPV infections resemble a common cold and may include:
- Cough: Often dry and persistent.
- Nasal Congestion: Stuffy or runny nose due to inflammation of the nasal passages.
- Fever: Usually low-grade, but can occasionally be higher in some cases.
- Sore Throat: Mild irritation or pain in the throat.
- Fatigue: General feeling of tiredness and malaise. These symptoms typically resolve on their own within 7–10 days without specific treatment
2.Moderate Symptoms
In some cases, particularly in children and older adults, the infection can progress to the lower respiratory tract, causing:
- Shortness of Breath: Difficulty breathing, especially during exertion.
- Wheezing: A whistling sound while breathing, often associated with airway inflammation.
- Headache: Generalized or sinus-related headaches caused by congestion.
- Body Aches: Muscle pain and discomfort, similar to flu-like symptoms.
3. Severe Symptoms
For vulnerable groups, such as infants, elderly individuals, and immunocompromised patients, hMPV can lead to serious complications involving the lower respiratory tract:
- Bronchiolitis: . Inflammation of the small airways (bronchioles). . Common in young children, presenting with rapid breathing, wheezing, and chest retractions.
- Pneumonia: .Inflammation of the lungs, causing fever, cough, chest pain, and difficulty breathing.
. Severe cases may require hospitalization and oxygen support.
- Hypoxia: Low oxygen levels in the blood due to impaired gas exchange in the lungs.
- Cyanosis: Bluish discoloration of the lips or skin, indicating severe respiratory distress.
4. Symptoms in High-Risk Groups
Infants and Young Children:
- Irritability, poor feeding, and lethargy are common non-specific symptoms.
- High risk of bronchiolitis and severe breathing difficulties.
Elderly Individuals:
- Exacerbation of pre-existing respiratory or cardiac conditions.
- Symptoms may include confusion or worsening of baseline health status.
Immunocompromised Patients:
- Prolonged symptoms and increased risk of secondary infections, such as bacterial pneumonia.
- May experience more severe and longer-lasting symptoms compared to others.
Duration of Symptoms
- Symptoms usually appear 3–6 days after exposure to the virus (incubation period).
- For mild cases, symptoms typically last 1–2 weeks.
- Severe cases may lead to prolonged illness, requiring several weeks for full recovery.
Differentiating hMPV Symptoms from Other Respiratory Viruses
hMPV symptoms overlap significantly with other common respiratory infections, such as:
- Respiratory Syncytial Virus (RSV): Both cause bronchiolitis and pneumonia, but RSV is more prevalent in younger children.
- Influenza: hMPV generally causes milder systemic symptoms (e.g., body aches and high fever).
- COVID-19: Loss of taste and smell, more specific to COVID-19, is not a hallmark of hMPV.
Laboratory testing (e.g., PCR) is often required to confirm hMPV infection, especially in cases with severe or ambiguous symptoms.
Complications of Untreated hMPV Infections
If left untreated, severe hMPV infections can lead to:
- Respiratory failure requiring mechanical ventilation.
- Hospitalization due to severe pneumonia or exacerbation of chronic illnesses.
- Secondary bacterial infections, such as sinusitis or bacterial pneumonia.
Recognizing the symptoms early is crucial, especially in high-risk populations, to prevent complications and ensure timely medical intervention.
Diagnosis of Human Metapneumovirus (hMPV)
Accurate diagnosis of human metapneumovirus (hMPV) is essential for proper management, especially in high-risk populations such as young children, the elderly, and immunocompromised individuals. However, diagnosing hMPV can be challenging due to its overlap with other respiratory viruses in terms of symptoms. Here’s an exploration of the methods used to identify hMPV infections.
Challenges in Diagnosis
- Non-Specific Symptoms: hMPV often mimics other respiratory infections like influenza, respiratory syncytial virus (RSV), or even COVID-19, making clinical diagnosis alone unreliable.
- Seasonal Overlap: hMPV infections typically peak in late winter and early spring, coinciding with outbreaks of other respiratory viruses, complicating differential diagnosis.
- Asymptomatic Cases: Some individuals, especially healthy adults, may experience mild or no symptoms but still carry and spread the virus.
For these reasons, laboratory testing is often required to confirm hMPV infection.
Diagnostic Methods
1. Molecular Testing (Gold Standard)
Polymerase Chain Reaction (PCR)
PCR is the most sensitive and specific method for detecting hMPV.
.It identifies the virus’s RNA in respiratory specimens such as:
Nasopharyngeal swabs
Throat swabs
Bronchoalveolar lavage (in severe cases).
Advantages:
- High accuracy:
- Can simultaneously detect multiple respiratory viruses using multiplex PCR panels.
Limitations:
- High cost and requires specialized equipment and expertise.
2. Antigen Detection
Immunofluorescence Assays (IFA):
- Detects viral antigens in respiratory epithelial cells.
- Respiratory specimens are stained with fluorescent antibodies that bind to hMPV antigens.
Advantages:
- Faster results than PCR.
- Useful in settings with limited molecular testing capabilities.
Limitations:
- Lower sensitivity compared to PCR.
- May produce false negatives in low viral load cases.
3. Viral Culture
- hMPV can be isolated in cell cultures, where its cytopathic effects (damage to cells) are observed.
Advantages:
- Useful for research and studying the virus’s behavior.
Limitations:
- Time-consuming (can take several days).
- Requires specialized laboratories and skilled personnel.
- Not commonly used in routine clinical settings.
4. Serology (Rarely Used for Acute Diagnosis)
- Measures antibodies (IgG and IgM) against hMPV in the blood.
- Useful for epidemiological studies or retrospective diagnosis.
Limitations:
- Not reliable for acute infections as antibodies take time to develop.
- Cross-reactivity with other viruses can lead to false positive
Treatment and Management of Human Metapneumovirus (hMPV)
Managing human metapneumovirus (hMPV) primarily involves supportive care, as there are no specific antiviral treatments currently available. The focus is on alleviating symptoms and preventing complications, especially in individuals at higher risk of severe illness. Here’s a detailed exploration of treatment and management strategies:
1. Supportive Care:Supportive care forms the cornerstone of hMPV management. It includes:
- Hydration: Ensuring adequate fluid intake to prevent dehydration, which is particularly important in young children and elderly patients.
- Symptom Relief: . Over-the-counter medications such as acetaminophen or ibuprofen can help reduce fever and alleviate pain. .Nasal saline drops or sprays and humidifiers can ease nasal congestion and improve breathing.
- Rest: Encouraging sufficient rest to support the body’s recovery. 2. Hospitalization for Severe Cases:
For individuals with severe respiratory symptoms or complications, hospitalization may be required. This is especially true for infants, elderly patients, and those with weakened immune systems. Hospital-based treatments may include:
- .Oxygen Therapy: Administered to patients with low oxygen levels to improve breathing.
- Mechanical Ventilation: In critical cases, ventilatory support may be necessary to manage respiratory failure.
- Intravenous Fluids: Provided to patients unable to maintain adequate hydration orally.
3. Management of Complications
Human metapneumovirus can lead to complications such as pneumonia or bronchiolitis, particularly in vulnerable populations. In such cases:
- Antibiotics: While antibiotics are not effective against viral infections, they may be prescribed to treat secondary bacterial infections.
- Bronchodilators: These may be used to relieve wheezing and improve airflow in patients with underlying asthma or other respiratory conditions.
4. Role of Antiviral Therapies
Currently, there are no antiviral drugs specifically approved for hMPV. However, ongoing research is exploring potential treatments targeting the virus. Experimental antivirals or monoclonal antibodies may become available in the future.
5. Prevention as Part of Management
Prevention plays a crucial role in reducing the burden of hMPV infections, particularly in high-risk groups. Preventive measures include:
- Hand Hygiene: Regular handwashing with soap and water.
- Respiratory Etiquette: Covering the mouth and nose when coughing or sneezing.
- Avoiding Crowded Spaces: Particularly during peak seasons of respiratory infections.
- Vaccination Research: Although no hMPV vaccine is currently available, efforts are underway to develop one.
6. Monitoring and Follow-Up
- Patients recovering from severe hMPV infections, especially those hospitalized, should have regular follow-ups to monitor for any lingering or recurring symptoms. Long-term effects are rare but may include prolonged respiratory issues in vulnerable individuals.
Conclusion
Human metapneumovirus (hMPV) and respiratory syncytial virus (RSV) share a close evolutionary relationship and significant clinical overlap. While RSV has historically been recognized as the leading cause of severe respiratory disease in children, hMPV has emerged as an important second contributor. Understanding their similarities and differences helps in improving diagnostics, treatment, and prevention strategies, ultimately reducing the global burden of respiratory infections.

Pingback: Most Important Frequently Asked Questions On hMPV Infection